David Robbins, MD is an internationally recognized leader in the minimally invasive surgical treatment of enlarged prostate. Dr. Robbins is a member of the Boston Scientific Strategic Advisory Board guiding the management of BPH surgery using the most modern and minimally invasive tools such as GreenLight laser and Rezum. Dr. Robbins is also the first urologist in South Florida certified to administer Aquablation for BPH. Dr. Robbins has taught GreenLight laser surgery in Peru, Chile, Colombia, and throughout the United States. He is the only certified GreenLight laser instructor in Florida. When it comes to optimal outcomes following BPH surgery, experience and expertise do matter.
What is the prostate?
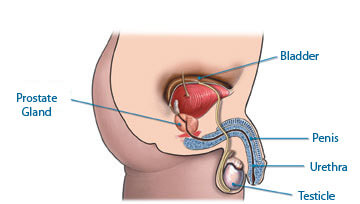
The prostate gland is a walnut-sized gland located in the male pelvis that sits between the bladder and the urethra just above the rectum. Urine passes through the prostate like a train through a tunnel as it passes into the male urethra during urination.
The exact function of the prostate is still largely unknown. The prostate contributes a small amount of fluid to the semen that assists the sperm to survive and navigate the female reproductive tract leading to the fertilization of an egg. The majority of the seminal fluid is contributed by the seminal vesicles which are grape-like sacs attached to the posterior surface of the prostate. The prostate does not play any role in sexual desire or erectile function.
What is Benign Prostatic Hypertrophy (BPH) or enlarged prostate?
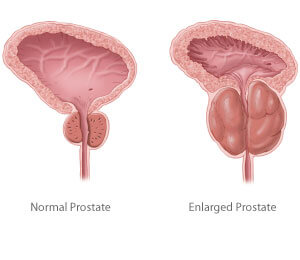
Benign Prostatic Hypertrophy (BPH) or enlarged prostate is also known as Benign Prostatic Growth or Benign Prostatic Enlargement. BPH is a non-cancerous enlargement of the prostate gland that affects more than 50% of men over the age of 60.
Although BPH (enlarged prostate) universally affects all aging males, it does so in varying degrees. Despite extensive basic science and clinical research on this subject, the pathogenesis of BPH remains poorly understood. What is clear is that BPH (enlarged prostate) is a complex disease with a multifactorial etiology involving both age and hormonal status.
There are two main periods of growth of the prostate. The first occurs during puberty when the prostate is known to double in size. The second period of growth begins in the third decade of life and continues throughout life eventually resulting in symptoms of BPH (enlarged prostate) in the aging male.
Why do some men have prostate problems and others do not?
All men who live past a certain age will develop BPH on a microscopic level, however, only 50% of these men develop macroscopic growth of the prostate meaning that they have a measurable physical increase in the size of the prostate.
Of those who have macroscopic BPH, only 50% will actually have clinical symptoms such as urgency, frequency, nocturia, decreased force of stream, difficulty initiating void and even incontinence.
It is interesting that there are some men with extremely large prostates with minimal symptoms and other men with very small prostates and highly bothersome symptoms.
How does the prostate cause symptoms in the aging male?
As the prostate enlarges, it slows down the flow of urine as it passes from the bladder to the urethra just like a kink in a garden hose. In the early phases of obstruction caused by the prostate, the patient experiences few symptoms because the bladder is able to compensate for increased resistance to the flow of urine by increasing the force of its contraction during urination. However, as the degree of obstruction increases, the patient begins to experience a host of symptoms that has come to be known as “prostatism” or “LUTS” (Lower Urinary Tract Symptoms). These bothersome symptoms are well known to that aging male and are typically the catalyst for making an appointment to see a urologist.
Symptoms of obstruction include decreased force of urinary stream, difficulty initiating urination, intermittent or prolonged urination, post-void dribbling, a sensation of incomplete emptying, the urgency of urination, urinary retention, and incontinence. Many of these symptoms can be attributed to changes that occur in the bladder as a result of having to force urine through an obstructed prostate. Similar to how skeletal muscle responds to increasing resistance and exercise, the smooth muscle of the bladder wall becomes stronger and thicker over time contracting with even minimal quantities of urine.
What are some potential medical consequences of BPH or enlarged prostate?
Urinary Retention
Urinary Retention is a situation that occurs when the obstruction from BPH (enlarged prostate) advances to the point when an individual can no longer empty his bladder because the prostate is literally blocking the urethra completely. This requires a trip to the emergency room to place a tube called a Foley catheter through the penis into the bladder that allows the urine to exit.
Bladder Stones
BPH (enlarged prostate) can result in an inability to completely empty the bladder so that there is always a residual amount of urine left in the bladder after voiding. This stagnant urine environment can allow for crystals in the urine to aggregate and form bladder stones of varying numbers and sizes. In extreme cases, these stones can fill up the entire bladder. Treatment options for this condition include open surgery to remove the stone or endoscopic surgery using cameras through the penis thereby allowing the use of lasers or ultrasonic energy to break up the stones.
Gross Hematuria (blood in the urine)
In certain circumstances, benign prostate growth can result in spontaneous bleeding resulting in blood-tinged urine or even large blood clots passing through the penis. Individuals on blood thinners such as Aspirin, Plavix, and Coumadin are more susceptible to spontaneous prostate bleeding. Nonetheless, anyone with gross hematuria requires a workup to rule out other possible causes including infection, stones, and cancer of the kidney, bladder, or prostate.
Urinary Tract Infections (UTIs)
Incomplete bladder emptying creates a more favorable environment for the growth of bacteria potentially resulting in a urinary tract infection.
How does a urologist evaluate a patient with BPH or enlarged prostate?
Flexible Cystoscopy
Flexible cystoscopy is a test in which a small flexible tube with a camera on the end is introduced into the bladder to allow the urologist to directly visualize the urethra, prostate, and bladder. This test is invaluable to the urologist in allowing him to visualize changes in the urinary tract that are associated with BPH (enlarged prostate). Prior to entering the bladder, the urologist will see the prostate. When the prostate is causing obstruction, the lateral lobes of the prostate that are normally separated may be seen touching each other or “kissing”. Additionally, there may be a median lobe, which is a component of the prostate not seen in all men that grow directly from the bladder neck at the 6 o’clock position. The median lobe, when enlarged can block the urethra like a ball-valve mechanism. Cystoscopy also allows for the evaluation of secondary changes in the bladder caused by obstruction from BPH. The bladder’s lining which is typically smooth becomes thickened as a result of the increased pressures needed to pass urine through an obstructed prostatic urethra. The urologist will see changes such as trabeculations (crossing muscular fibers), cellules, and even a diverticulum (a large outpouching of the bladder lining). Cystoscopy is an office-based procedure that typically takes less than 5 minutes to perform and generally causes minimal discomfort to the patient.
Uroflow
Uroflow is a simple test used to measure the flow rate of urine during voiding. A device is used to measure the flow of urine and a computer plots a curve of volume per time. A flow of fewer than 10 ccs/sec is considered consistent with obstruction. There are several confounding factors that influence the results of this test, but its benefits are significant in that it is easy to perform and completely non-invasive.
Urodynamics
This test can be employed for men with symptoms of BPH that are not responding to medical therapy and are considering surgical intervention. This test allows the urologist to make objective measurements of the true bladder pressure and flow rate as it is measured in real-time. The test typically takes 15-30 minutes to perform and involves the placement of a small catheter in the bladder used to measure bladder pressure and a small catheter in the rectum used to measure intra-abdominal pressure.
Urocuff™ Study for BPH
At Urological Consultants of Florida, we are one of the few centers in the Miami region that offer our patients a minimally invasive option for measuring the pressure-flow relationship typically only demonstrated via a urodynamic evaluation.
Urocuff™ is the first non-invasive test that can accurately identify good surgical candidates and provide an objective basis for managing Flomax and similar medications. Many men who have been reluctant to undergo the catheterization necessary for conventional urodynamics can now be tested quickly and comfortably.
The Urocuff machine uses a method similar to that for blood pressure measurement. A penile cuff (similar to a blood pressure cuff) is fitted to the patient who is then asked to void in the normal way. An estimate of bladder pressure and measurement of maximum flow rate are obtained and plotted on a nomogram to allow categorization into obstructed, not obstructed, or “diagnosis uncertain” groups.
Medical and Surgical Treatments for Enlarged Prostate (BPH)
There are various treatments for BPH that are highly dependent on patient factors such as age, duration of urinary symptoms, prior urological treatment, and comorbid medical conditions. The two basic treatment algorithms include medical and surgical therapy.
Surgical treatment for BPH is always a secondary option and is only considered when medical therapy has been attempted but has not alleviated the symptoms of benign prostatic hyperplasia sufficiently to allow for the patient to have a satisfactory quality of life with regard to his urinary symptoms. The principal focus of surgical therapy is to eliminate prostate tissue with the goal of relieving obstruction from the prostate and improving the flow of urine as it exits the bladder.
GreenLight Laser Surgery
GreenLight Laser Surgery is a minimally invasive outpatient surgical option for BPH (enlarged prostate) that is performed using a video camera placed in the urethra without the need for a surgical incision. GreenLight Laser surgery combines the effectiveness of the traditional surgical procedure known as transurethral resection of the prostate (TURP), but with fewer side effects, shorter catheterization, and a quicker, less painful recovery.
Suprapubic/Retropubic Prostatectomy
Before the invention of medical therapy for BPH and endoscopic therapies with cameras, the only option for the treatment of urinary obstruction from BPH was an open suprapubic or retropubic prostatectomy. This surgery consists of making a large incision into the patient's belly, opening a hole in the bladder, incising the capsule of the prostate, and literally using a finger to shell out the entire prostate. While considered very effective, this surgery could be associated with bleeding, a prolonged hospital course, and the need to leave a foley catheter or suprapubic tube for an extended period of time. Although this procedure is performed infrequently nowadays with the invention of medical therapy and endoscopic surgical options such as TURP and Green Light laser, it is still the most effective method for treating BPH in patients with prostates that are extremely large.
Transurethral Resection of the Prostate (TURP)
With the invention of surgical cameras or “telescopes”, the TURP became the gold standard of care and has remained that way for many years. During a TURP, the urologist uses an electrical loop attached to the end of a surgical camera to shell out small pieces of prostate tissue and clear a channel in the prostate. TURP has an excellent success rate and is certainly less invasive than an open prostatectomy. However, TURP does have some drawbacks and potential complications. First of all, the tissue bleeds as it is cut leading in some patients to the need for blood transfusions or a prolonged hospital stay waiting for the bleeding to stop. The electrical energy using during a TURP could also injure the nerves around the prostate that cause erections potentially leading to erectile dysfunction. Additionally, one of the biggest concerns during a TURP is “TUR Syndrome” which is an electrolyte disturbance involving sodium that occurs when the body absorbs glycine. Glycine is the irrigation fluid that is used during a TURP which is beneficial in that it allows the conduction of electricity needed to perform a TURP, however, it has less sodium than the body, and when absorbed it can dilute the sodium level in the body and cause potentially dangerous side effects such as altered mental status and loss of consciousness. Additional potential side effects from TURP include urethral stricture, bladder neck contracture, urge incontinence, and retrograde ejaculation.
Medical therapy including alpha-blockers and 5 alpha-reductase inhibitors
Soon after the invention of the TURP, it was not long before the drug companies entered the market of BPH therapy. The first medications on the market were alpha-blockers which are a class of medications that relax the smooth muscle component of the prostate. They improve voiding symptoms and flow by making the hole in the prostate less tight, however, they do not decrease the mass of the prostate or diameter of the hole like surgical therapies do. The first alpha-blockers on the market were Hytrin and Cardura. Newer medications on the market include Flomax, Uroxatral, and Rapaflo. Possible side effects of these medications include retrograde ejaculation and dizziness. Retrograde ejaculation is a decreased or absent ejaculation during orgasm and is caused by the prevention of closure of the bladder neck during ejaculation.
5 alpha-reductase medications such as Proscar and Avodart are often used in conjunction with alpha-blockers especially in men with larger-sized prostates. These medications block the conversion of testosterone to dihydrotestosterone which is the active form of testosterone that causes prostate growth. These medications literally shrink the size of the prostate up to 50% by six months. In conjunction with alpha-blockers, these medications can synergistically improve symptoms and decrease the risk of complications of BPH such as urinary retention, prostate bleeding, and the need for surgical therapy.
Request Your Consultation Today!
To request your consultation, please call (305) 575-2771 or contact us online today!
Our Locations
12411 Biscayne Boulevard
North Miami, FL 33181
Phone: (305) 575-2771
Get Directions







